What is Telehealth?
Telehealth basically means using digital tools like your phone, tablet, or computer, to connect with your doctor and manage your health without having to be there in person. Sometimes you use it from home and other times a nurse or health professional might use it from a clinic,, especially in rural or hard-to-reach areas. It also includes the behind-the-scenes technology your care team uses to streamline and support your treatment.
Telehealth, often called e-health or m-health, is designed to do things like:
• Make it easier for people in remote or rural areas to get care
• Keep everyone safer during outbreaks or infectious illnesses like COVID-19
• Provide everyday primary care for a wide range of conditions
• Help people who have limited mobility or transportation get the services they need
• Give quicker access to specialists
• Improve communication and coordination among your health care team
• Offer guidance so you can better manage your own health
A lot of people started using telehealth during the pandemic and realized how convenient it is. So, it has continued to grow and become a bigger part of everyday health care.
Advantages:
• Telehealth saves time and money:
One of the biggest benefits of telehealth is how much it cuts down on unnecessary travel. Patients do not have to spend hours on the road or pay for transportation just to see a doctor. A quick virtual check-in often replaces a full trip. This makes care a lot more convenient and affordable.
• Doctors get real-time patient data:
Telehealth tools let doctors receive important readings like blood pressure, glucose levels, or oxygen saturation from patients at home. This regular flow of information helps them make accurate and fast decisions instead of waiting weeks for an in-person appointment.
• Remote patient monitoring supports long-term care:
Remote patient monitoring (RPM) has become essential. Especially with health systems moving toward value-based care. These tools help patients stick to their treatment plans and flag early warning signs. It ultimately leads to better outcomes and fewer hospital visits.
• Virtual visits make providers more efficient:
For physicians, telehealth helps organize schedules more smoothly. It reduces the number of missed appointments and allows doctors to see more patients. Avoiding the downtime that typically comes with in-person visits.
• Patients benefit from less stress and fewer expenses:
Beyond saving travel time, telehealth also reduces the stress of taking time off work or arranging childcare. For many people, a 15-minute virtual visit is far more manageable than spending half the day at a clinic.
• A lifeline for rural and underserved communities
Telehealth is especially powerful for people who live far from a hospital or face shortages of specialists. It bridges the gap by making quality care available to people who would otherwise have to travel hours for the same treatment.
• Research shows it reduces costs and unnecessary hospital use
According to a report from the Institute of Medicine, telehealth has helped rural hospitals reduce preventable readmissions and emergency room visits. That means lower costs for both patients and healthcare systems.
• Adoption has surged over the past decade
Telehealth has grown rapidly. From about 35% of U.S. hospitals offering some form of virtual care ten years ago to roughly 76% today. That jump shows how quickly remote care has moved from being optional to almost standard.
• COVID-19 accelerated its importance
During the pandemic, telehealth became a safe alternative to in-person visits. Many people preferred virtual appointments to avoid exposure, and that shift pushed telehealth into the mainstream faster than anyone expected.
Challenges:
• Limited digital access:
Not everyone has a fast internet connection or the confidence to use digital tools. This digital gap affects both patients and providers. It makes it hard for some people to fully benefit from telehealth services.
• Low patient engagement:
Virtual visits can feel less personal. Without face-to-face interaction or body language cues, patients may feel less connected. This can lead to missed appointments or less willingness to open up during a session.
• Privacy concerns:
Keeping patient information secure is a major challenge. Telehealth platforms need strong cybersecurity and providers must follow strict regulations. Any weak point puts sensitive data at risk.
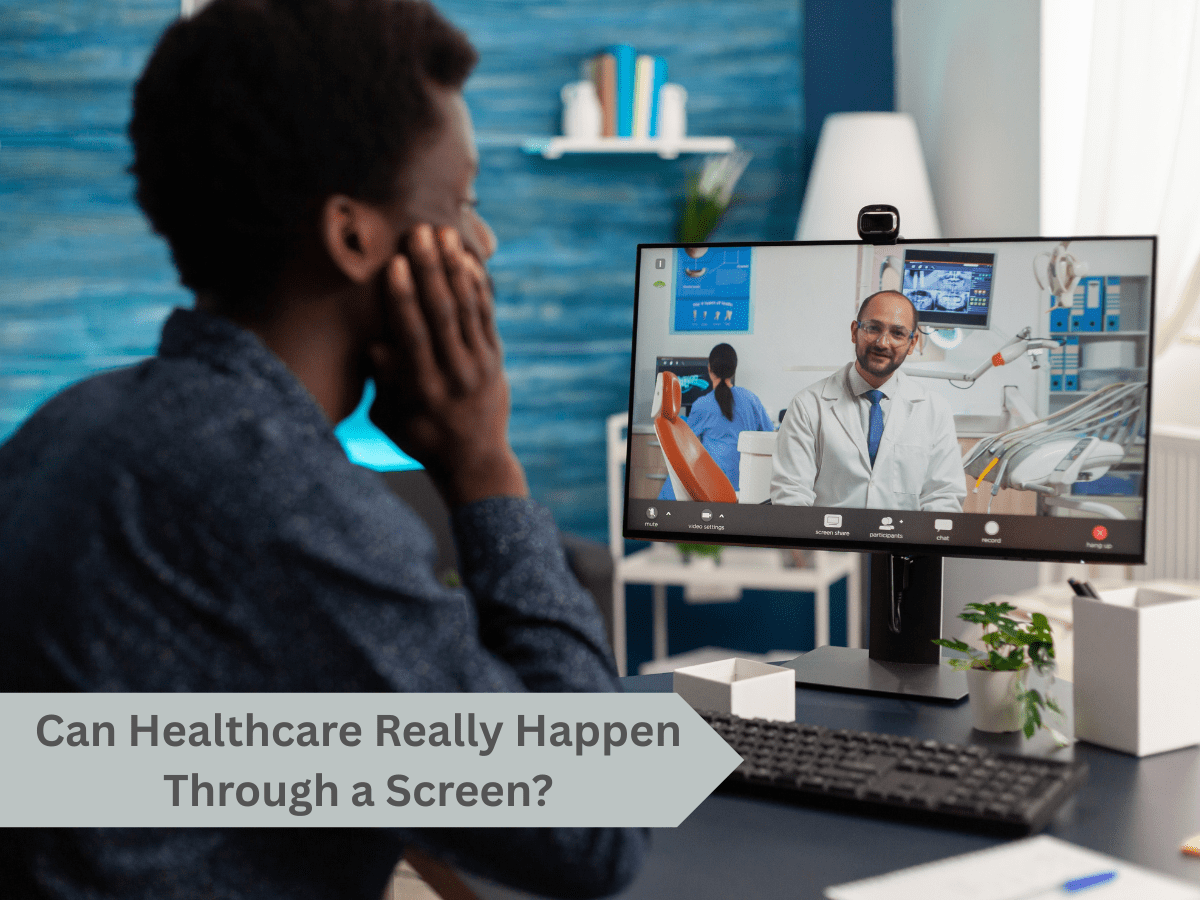
• Clinical limitations:
Telehealth is not a complete replacement for in-person care. Certain conditions require physical exams, procedures, or diagnostic tests that simply can’t be done through a screen.
• Workflow disruptions:
Poor integration between telehealth tools and existing clinic systems can create scheduling conflicts and communication delays. This disrupts the flow of both administrative and clinical work.
• Licensing and reimbursement issues:
Different states and regions have their own rules about who can provide telehealth care and how much insurance will cover. These inconsistent policies slow down adoption and make it harder for doctors to treat patients across borders.
• Low satisfaction for some users:
When people struggle with unfamiliar platforms or run into technical problems, it reduces their confidence in virtual care. This can make telehealth feel frustrating rather than convenient.
• Technical failures:
Dropped calls, frozen screens, lag in videos, and app crashes interrupt appointments and weaken trust in digital care. Even small glitches can derail a consultation.
While telehealth comes with its share of challenges, they are not insurmountable. With the right tools and systems in place, clinics can boost patient engagement and make their operations run smoothly.

References:
https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/telehealth/art-20044878
https://telehealth.hhs.gov/patients/why-use-telehealth
https://www.health.harvard.edu/staying-healthy/telehealth-the-advantages-and-disadvantages
https://www.healthrecoverysolutions.com/blog/common-telehealth-challenges-and-how-to-overcome-them